3 May 2024
6 min read
Is your NHS prescribed pulmonary function test ‘safe and effective’?
A 37 year old male patient with a history of cannabis and tobacco smoking presents with a persistent cough of over 6 months duration. He works in the local paint factory and has 'had all the tests' from the GP and in hospital for the cough. In order of invasiveness (where 1=hardly and 5=very invasive) suggest which tests he may have already had performed.
The allopathic medicine practitioners would most likely blame his smoking on his chronic cough, rather than the exposure to toxins in the paint factory he works at.
The most important component of paints is solvents. Solvents have been shown to affect critical systems in the body; auditory system, central nervous system, hepatic system, renal system, and respiratory system. Exposure through inhalation is the most common route of entry into the body. There is a current study ongoing among paint factory workers in Mauritius, since incidence of respiratory diseases have been on the rise among the paint factory workers in the past 5 years. [1]
Pulmonary function tests include:
Spirometry: this test measures how much air you can breathe in and out of your lungs, as well as how easily and fast you can blow the air out of your lungs. During the test, you will be sitting upright. A clip is placed on your nose and you will be given a plastic mouthpiece connected to the spirometry machine. You will place your lips tightly around the mouthpiece and be asked to take in as big and deep a breath as possible and then blow out as hard and fast as you can. This maximal effort is very important, and testing will be repeated at least three times to get the best results.
The technician may give you a medicine (metacholine) to help open your airways and then repeat the test to see if your breathing improves with the medicine. The testing takes about 30 to 45 minutes. [2]
Metacholine mimics the neurotransmitter acetylcholine to directly interact with muscarinic receptors on airway smooth muscle, resulting in contraction and airway narrowing. This occurs at a lower inhaled dose and to a greater degree in individuals with asthma or AHR than in those with normal airway responsiveness. Similar direct airway responses can be demonstrated with histamine.
Bronchoconstriction can also be elicited through exercise or other stimuli to the airways that act indirectly to cause airway narrowing. Both exercise and eucapnic hyperventilation (exercise induced asthma) cause airway drying and cooling, and the stimulus to bronchoconstriction is now recognised to involve the osmolar change in the airway epithelium resulting from water loss. [3]
The side effects of metacholine incl.: headache, sore throat, light-headedness, nausea, vomiting, or dizziness. Serious side effects incl. trouble breathing, cough, wheezing, chest pain/tightness and irregular heartbeat. A very serious allergic reaction can also occur. [4]
Considering that the administration of metacholine can cause bronchoconstriction and induce and asthma attack, wheezing or shortness of breath, and cough- the very same thing the man came to investigate, I would not say the test is benign at all, hence I'd rate it as a 3 qua invasiveness.
CT scan (computed tomography scan)
CT scan refers to a computerized x-ray imaging procedure in which a narrow beam of x-rays is aimed at a patient and quickly rotated around the body, producing signals that are processed by the machine's computer to generate cross-sectional images, or “slices.” These slices are called tomographic images and can give a clinician more detailed information than conventional x-rays. Once a number of successive slices are collected by the machine's computer, they can be digitally “stacked” together to form a three- dimensional (3D) image of the patient that allows for easier identification of basic structures as well as possible tumors or abnormalities. Unlike a conventional x- ray—which uses a fixed x-ray tube—a CT scanner uses a motorized x-ray source that rotates around the circular opening of a donut-shaped structure called a gantry. [5] CT scans use x-rays, and all x-rays produce ionizing radiation. Ionizing radiation has the potential to cause biological effects in living tissue. Currently, AI is being trained to interpret the effects of COVID.
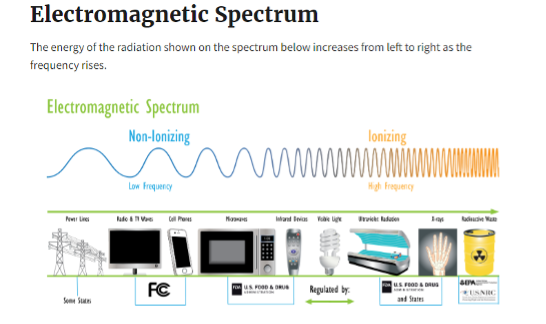
There are two kinds of radiation: non-ionizing radiation and ionizing radiation.
Non-ionizing radiation has enough energy to move atoms in a molecule around or cause them to vibrate, but not enough to remove electrons from atoms. Ionizing radiation has so much energy it can knock electrons out of atoms, a process known as ionization. Ionizing radiation can affect the atoms in living things, so it poses a health risk by damaging tissue and DNA in genes. Ionizing radiation comes from x-ray machines, cosmic particles from outer space and radioactive elements. Radioactive elements emit ionizing radiation as their atoms undergo radioactive decay. Gamma rays (Y) are weightless packets of energy called photons. Unlike alpha and beta particles, which have both energy and mass, gamma rays are pure energy. Gamma rays are similar to visible light, but have much higher energy. Gamma rays are often emitted along with alpha or beta particles during radioactive decay.
Gamma rays are a radiation hazard for the entire body. They can easily penetrate barriers that can stop alpha and beta particles, such as skin and clothing. Gamma rays have so much penetrating power that several inches of a dense material like lead, or even a few feet of concrete may be required to stop them. Gamma rays can pass completely through the human body; as they pass through, they can cause ionizations that damage tissue and DNA. X-rays and gamma rays have the same basic properties but come from different parts of the atom. X-rays are emitted from processes outside the nucleus, but gamma rays originate inside the nucleus. They also are generally lower in energy and, therefore less penetrating than gamma rays. X-rays can be produced naturally or by machines using electricity.
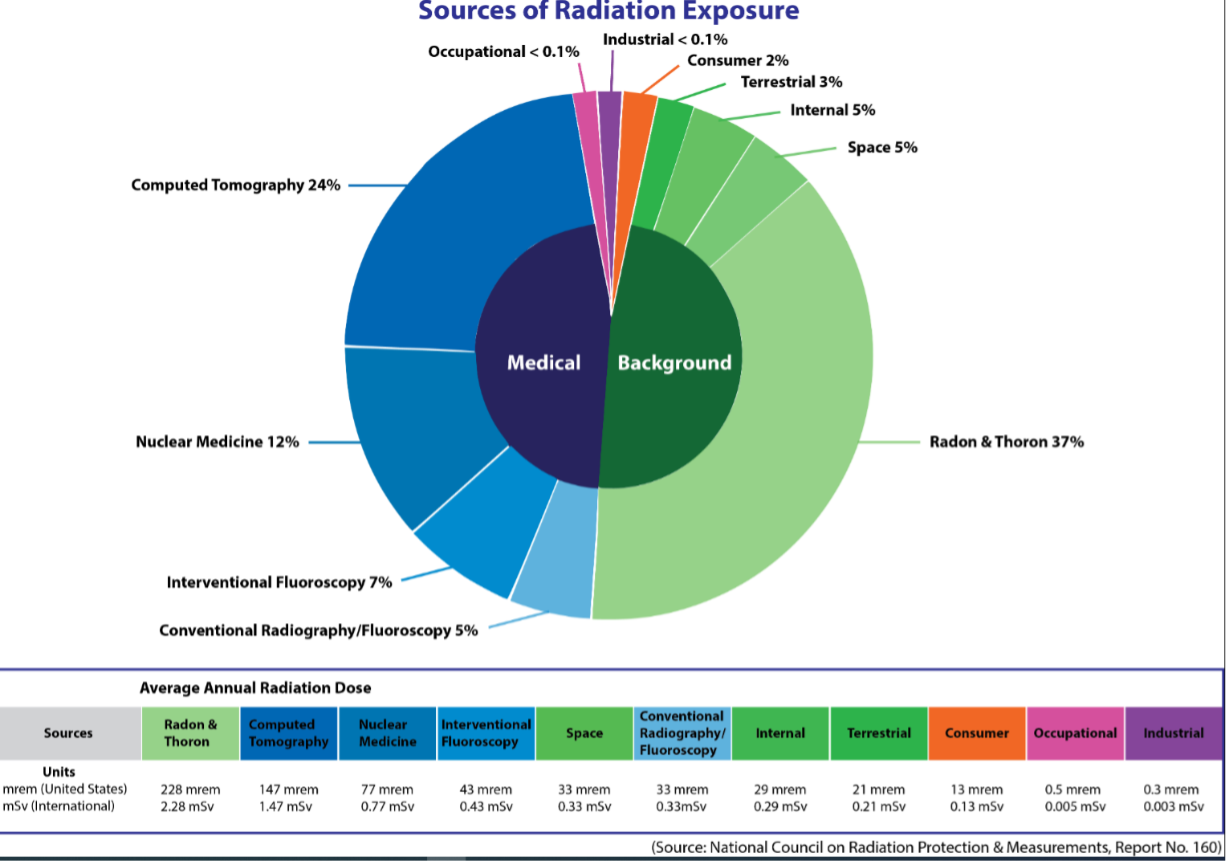
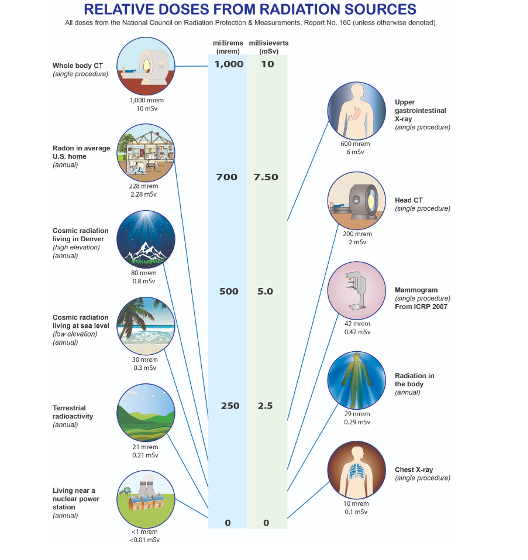
So how much ionizing radiation does a CT scan provide?
There are four different but interrelated units for measuring radioactivity, exposure, absorbed dose, and dose equivalent. These can be remembered by the mnemonic R-E-A-D.[7]
Radioactivity refers to the amount of ionizing radiation released by a material. Whether it emits alpha or beta, gamma or x-rays, or neutrons, the quantity of radioactive material is expressed in terms of its radioactivity, which represents how many atoms in the material decay in a given time period. The units of measure for radioactivity are the curie (Ci) and becquerel (Bq). Exposure describes the amount of radiation travelling though the air. Exposure is measured in roentgen (R) and coulomb/kilogram (C/kg). Absorbed dose describes the amount of radiation absorbed by an object or person. The units for absorbed dose are the radiation absorbed dose (rad) and gray (Gy). Dose equivalent (or effective dose) combines the amount of radiation absorbed and the medical effects of that type of radiation. For beta and gamma radiation, the dose equivalent is the same as the absorbed dose. By contrast, the dose equivalent is larger than the absorbed dose for alpha and neutron radiation, because these types of radiation are more damaging to the human body. Units for dose equivalent are the roentgen equivalent man (rem) and sievert (Sv), and biological dose equivalents are commonly measured in 1/1000th of a rem (known as a millirem or mrem). For practical purposes, 1 R (exposure) = 1 rad (absorbed dose) = 1 rem or 1000 mrem (dose equivalent).
Note that a measure given in Ci tells the radioactivity of a substance, while a measure in rem (or mrem) tells the amount of energy that a radioactive source deposits in living tissue.
About 48% of the average American's radiation dose comes from medical procedures, this does not include radiation therapy used in the treatment of cancer, which is typically many times larger. Also, when we add occupational, industrial and consumer radiation exposure to this, we get 50, 02%, which is just over the half of human-made radiation received vs. 'natural' radiation we are exposed to.
The primary U.S. limit for occupational exposure to ionizing radiation is 5,000 mrem (50 mSv)/year. Exposure to minors and to the general public is limited to 100 mrem (1 mSv)/year.[10] Allopathic medicine practitioners tend to argue that the benefit of detecting a disease outweighs the level of ionizing radiation received. Cancers caused by radiation exposure cannot be distinguished from those caused by other environmental, chemical, or biological factors. Cancers that might develop from a radiation exposure usually have a latency period of 2 to 10 years after the exposure. Hence, I presented the facts, so that my patients can make up their own minds based on informed consent. Invasiveness: 1, lethality potential 5.
Xray
Is often used post-bronchoscopy, yet are deemed to rarely provide actionable information for patients without acute symptoms and expose patients to potentially unnecessary radiation. (Pls. see information discussed under CT scan). Invasiveness: 1, lethality potential 5.
Bronchoscopy
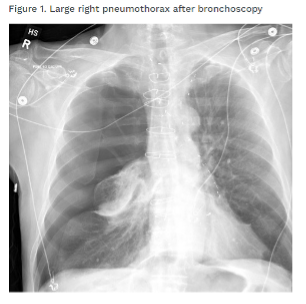
Bronchoscopy is a technique used to look at your air passages with a small camera that is located at the end of a flexible tube. This connects to a video screen for the doctors to view and take photos of your air passages. The tube also has a small channel to collect tissue samples from your lung that can be used in disease diagnosis. This procedure can also be done with the assistance of a robot [11]. A Norwegian study [12] on the bronchoscopy complication rates has shown, that bleeding varies from 2.5% to 100% of procedures; desaturation from 0.7% to 76.3% of procedures and fever in 2% to 33% of procedures. An early termination of bronchoscopy was required in 25.9% of the cases. 3 subjects (1.3%) experienced potentially severe complications. Sample size was 239. Prior to the procedure, the patient is sedated, usually with Alfentanil. It is a synthetic, short-acting opioid analgesic- a derivative of fentanyl. It is used as an option for dying who can't tolerate morphine due to renal failure. A numbing spray is used to relax mouth and throat. The throat may be numb for an hour after the procedure. Medications provided to induce various levels of sedation (from light to general anesthesia) can have hemodynamic consequences including hypotension and arrythmias in the peri-procedure period [13]. Sore throat, post-procedural cough (in 55% of patients) or hoarseness may last for the next 24 hours. Risks incl. a hole in your airway, irritation of inflammation of vocal cords and iatrogenic pneumothorax (lung collapse). Apparently, the incidence rate for the latter is 0.16% when bronchoscopy alone is performed and up to 20-30% after placement of endobronchial valves (used as a treatment for COPD and emphysema). [14]
I am rating bronchoscopy as a 4 qua invasiveness and safety. Here are British Thoracic Society's guidelines for diagnostic flexible bronchoscopy in adults https://thorax.bmj.com/content/68/Suppl_1/i1.
(Post-procedural or endobronchial) ultrasound
Lung ultrasound (LUS) is a widely available technique allowing rapid bedside detection of different respiratory disorders. Its reliability in the diagnosis of community-acquired lung infection has been confirmed. However, its usefulness in identifying infections caused by specific and less common pathogens (e.g., in immunocompromised patients) is still uncertain. To be detected from LUS, a parenchymal lesion must be close enough to the pleura. 'In patients with typical bacterial pneumonia, the parenchymal consolidation usually appears as a sub-pleural hypo-echoic area associated with hyper-echoic dynamic spots called “air bronchograms”, representing air-filled bronchi within the density of surrounding alveoli. The pleural line above the consolidation is less echogenic or even non-visible [15]. So the usefulness of LUS in the detection of bacterial pneumonia is next to 0. Ultrasonic waves are waves of frequency above the audible frequencies of the human ear. Ultrasonic waves are mechanical waves with a frequency greater than 20,000 Hz. Those waves are of higher frequency and shorter wavelengths. (Imagine calm waves vs. storm waves). Ultrasound waves can heat the tissues slightly and produce small pockets of gas in body fluids or tissues. Babies exposed to ultrasound scans can be born with lower birth weight, dyslexia, delayed speech, and non-right-handedness. Experiments on animals have shown damage to internal organs from receiving different ultrasonic frequencies. [16]
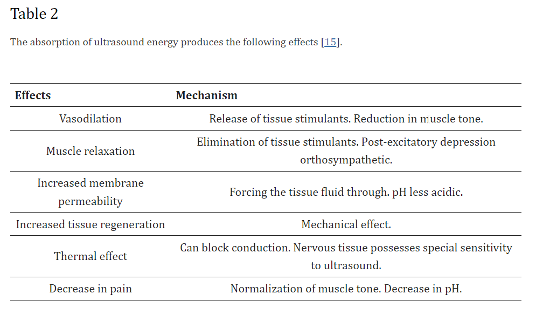
An analysis of 114 recent studies on the effects of ultrasound on a living body have noted the following effects: vasodilation, muscle relaxation, increased membrane permeability, increased tissue regeneration, thermal effect and decrease in pain.
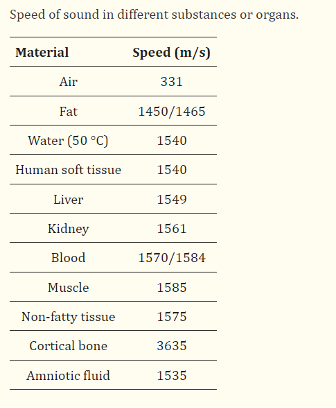
'For most diagnostic beams, 90% of the power is deposited within the first 5 cm of tissue. Essentially all the acoustic power entering through the skin surface is absorbed in the body tissues. Speed through tissue depends on fat, collagen and water content. Ultrasounds cause an increase in the speed of biochemical reactions by increasing temperature.' The speed of sound is highest in the cortical (dense) bone: 3635 m/sec.
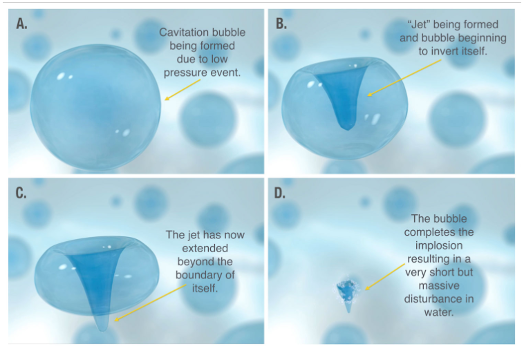
One of the effects of ultrasound is called 'cavitation'- phenomena which produce the creation, oscillation, growth and shock of bubbles within a medium. Basically, bubbles are formed, which grow and then explode, resulting in cell death (lysis), breakage of the cell membrane and the release of its contents. [17]
An example of this is non-surgical liposuction. Even though labelled as 'safe & effective', I will rate this one as 3 qua invasiveness.
Plethysmography
Body plethysmography allows to assess functional residual capacity (FRCpleth) and specific airway resistance (sRaw) as primary measures. In combination with deep expirations and inspirations, total lung capacity (TLC) and residual volume (RV) can be determined. Side effects incl. dizziness and coughing. During the test the cubicle may become very warm, as well as some people may feel claustrophobic. Rare complications incl. collapsed lung, retinal detachment, heart attack in patients with previous cardiac disease, sudden changes in blood pressure, stroke and airway narrowing. Invasiveness: 2. Is often used post-bronchoscopy, yet are deemed to rarely provide actionable information for patients without acute symptoms and expose patients to potentially unnecessary radiation. (Pls. see information discussed under CT scan). Invasiveness: 1, lethality potential 5.
Exhaled Nitric Oxide Test
This test measures the amount of nitric oxide that is exhaled from a breath. Increased level of nitric oxide is associated with swelling of lung airways. This test can be used to determine whether someone being treated for asthma is responding well to certain medications. The results indicate if an asthmatic should take steroids or other medication, as well as assess the effects of current medication. 1 for invasiveness.
Conclusion
Informed consent means, you have been provided with sufficient information to know what you are buying into. We spend more time researching the cars and yoga pants we want to purchase, than the diagnostics or drugs the NHS wants us to subscribe to. Above info is available and accessible for all- still. I hope you will make informed decisions.
Author: Evelin Kallas
References
- 1. National Library of Medicine,. 'Study protocol to determine the effects of solvents on lung function among paint industry workers in Mauritius: A cross-sectional study' (29 April 2024). [website] Link
- 2. American Lung Association. 'What is Spirometry and Why It is Done' (29 April 2024). [website] Link
- 3. A.L. Coates et al.,. 'ERS technical standard on bronchial challenge testing: general considerations and performance of methacholine challenge tests' (). European Respiratory Journal, Vol. 49, Issue 5, 2017.
- 4. Heath Link British Columbia. 'Metacholine-Inhalation ' (29 April 2024). [website] Link
- 5. United States Environmental Protection Agency,. Radiation Sources and Doses (30 April 2024). [website] Link
- 6. United States Environmental Protection Agency,. Radiation Sources and Doses (30 April 2024). [website] Link
- 7. Department of Energy,. Radiation in Perspective (30 April 2024). [website] Link
- 8. United States Environmental Protection Agency,. Radiation Sources and Doses (30 April 2024). [website] Link
- 9. United States Environmental Protection Agency,. Radiation Sources and Doses (30 April 2024). [website] Link
- 10. Department of Energy,. Radiation in Perspective (30 April 2024). [website] Link
- 11. American Lung Association,. Bronchoscopy (29 April 2024). [website] Link
- 12. E. Orvedal Leiten et al.,. 'Complications and discomfort after research bronchoscopy in the MicroCOPD study' (). BMJ Open Respiratory Research, Vol 7, Issue 1, 2022.
- 13. Patient Safety Network: Agency for Healthcare Research and Quality,. False Assumptions Result in a Missed Pneumothorax after Bronchoscopy with Transbronchial Biopsy (30 April 2024). [website] Link
- 14. Patient Safety Network: Agency for Healthcare Research and Quality,. False Assumptions Result in a Missed Pneumothorax after Bronchoscopy with Transbronchial Biopsy (30 April 2024). [website] Link
- 15. National Centre for Biotechnology Information,. The Role of Ultrasound in the Diagnosis of Pulmonary Infection Caused by Intracellular, Fungal Pathogens and Mycobacteria: A Systematic Review (01 May 2024). [website] Link
- 16. National Centre for Biotechnology Information,. Possible Effects on Health of Ultrasound Exposure, Risk Factors in the Work Environment and Occupational Safety Review (01 May 2024). [website] Link
- 17. Getinge,. What is cavitation? (01 May 2024). [website] Link